Ankylosing spondylitis (Bechterew’s disease)

Introduction: In this article we will provide an in-depth description of Ankylosing Spondylitis. You will gain an understanding of the nature of the disease, its causes and symptoms as well as the importance of physical activity, exercises and fascial therapy to manage the disease and improve the quality of life of people living with ankylosing spondylitis.
What is ankylosing spondylitis?
Ankylosing spondylitis (AS), formerly known as Bechterew’s disease, is an autoimmune, chronic inflammatory disease that mainly affects the joints of the spine and the pelvic joints (sacroiliac joints). The disease is characterized by inflammation, aching pain and progressive stiffness of the spine. The most common age of onset of ankylosing spondylitis is usually adults between the ages of 20 and 40, but it can also occur in older people and, in rare cases, in children.
Causes of ankylosing spondylitis:
The causes of ankylosing spondylitis are not yet fully understood, but there is a strong link to genetic factors, particularly the HLA-B27 gene. People with the HLA-B27 gene are more likely to develop the disease, but this is not an absolute indication that they will be affected. There is also an autoimmune component where the body’s immune system mistakenly attacks its own tissues, leading to inflammation and degenerative changes.
Symptoms of ankylosing spondylitis:
It is common for AS to start with pain and discomfort in the lower spine and pelvis. The symptoms come on gradually over time and eventually lead to stiffness in the back with reduced mobility over time. It is common to experience lower back pain and stiffness in the morning or after periods of inactivity.
Diagnosis and treatment of ankylosing spondylitis:
Ankylosing spondylitis is diagnosed when the patient meets four out of five specific criteria for AS, but physical examination and imaging tests such as X-rays and MRI can also be used. It is important to diagnose the disease early in order to provide adequate treatment and reduce the risk of long-term complications.
The treatment of ankylosing spondylitis aims to reduce inflammation, relieve pain, improve mobility and prevent or delay progressive stiffness of the spine. Medication plays an important role in treatment and can include non-steroidal anti-inflammatory drugs (NSAIDs), immunomodulatory drugs and biologics that target the inflammatory process. Physiotherapy and exercise are also important components of treatment to improve mobility, strength and flexibility of the spine and surrounding muscles.
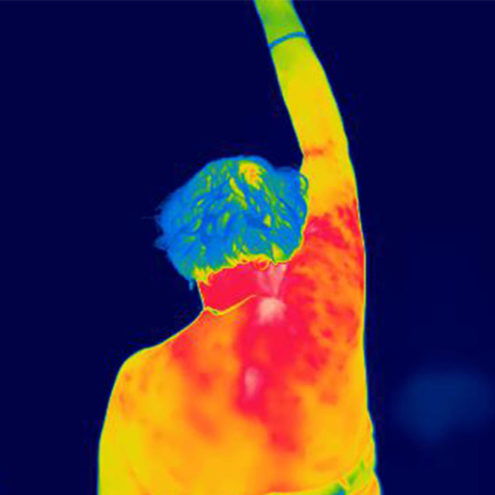
Fascia treatment for the relief of ankylosing spondylitis symptoms: Fascia treatment, performed by certified fascia specialists at the the FasciaClinics, can be an effective complementary treatment method for people with ankylosing spondylitis. Fascia is the network of connective tissue that surrounds and connects muscles, joints and organs in the body. Through specific techniques, fascia specialists can help release tension and increase mobility in the fascia around the spine. This can lead to pain relief, improved circulation, better mobility and a straighter posture.
Frequently asked questions about ankylosing spondylitis:
Here are some common questions that people with ankylosing spondylitis may have:
What is the difference between ankylosing spondylitis and regular back pain?
Ankylosing spondylitis differs from ordinary back pain by its inflammatory nature and gradual loss of mobility in the spine. Back pain can be an early symptom of ankylosing spondylitis, but the disease usually involves more than just pain and can lead to stiffness and difficulty moving.
Can ankylosing spondylitis be cured?
Unfortunately, there is no cure for ankylosing spondylitis. It is a chronic disease that usually lasts a lifetime. However, with early diagnosis and adequate treatment, symptoms can be relieved and the progression of the disease can be prevented or delayed.
What are the best treatment options for ankylosing spondylitis?
Treatment options for ankylosing spondylitis can vary depending on individual needs and symptoms. Common treatment approaches include medication to reduce inflammation and pain, physiotherapy to improve mobility and strength in the muscles, and lifestyle changes such as exercise, good posture and relaxation techniques.
How can I relieve pain and improve back mobility in ankylosing spondylitis?
Regular exercise and physical activity are important to relieve pain and improve mobility in ankylosing spondylitis. Specific exercises that stretch and strengthen the back and trunk muscles can be particularly beneficial. Heat treatment, such as hot showers or warm compresses, can also help relieve pain and increase mobility.
How does ankylosing spondylitis affect quality of life and how can it be managed?
Ankylosing spondylitis can have a significant impact on quality of life by limiting mobility and causing pain. To manage the disease, it is important to follow an individualized treatment plan that includes medication, exercise, correct posture and ergonomic adjustments in everyday life. Getting support from health professionals, joining support groups and learning relaxation techniques can also help manage the physical and emotional challenges that can arise.
Advice from a fascia specialist
It is important to consult a certified fascia specialist for advice and to design an individual treatment plan. Be sure to follow their advice and customize the treatment according to what feels most comfortable and effective for you.
In conclusion, ankylosing spondylitis is a disease that can affect the quality of life of those who suffer from it. By understanding the disease and applying appropriate treatment strategies such as medication, exercise and fascia therapy, you can relieve pain, improve mobility and live a more active and comfortable life. Remember to consult a fascia specialist for individual advice and support during your treatment journey.
 Search
Search